If you caught the newscast a couple of weeks ago, you might be wondering: Why two radiation treatments? I sat down with the radiation docs a few days ago to get a full explanation, which means it’s time once again to play Short Answer, Long Answer.
Short Answer
One treatment is for the pancreas, and one is for the liver.
Long Answer
Radiation treatment has historically been “external beam”, which means that high-energy x-rays are aimed into the patient’s body from an outside machine. The hope is that the radiation kills cancer cells without damaging healthy tissue. This has always been tricky when the cancer is in the abdomen, as that whole area moves around a lot with every breath. So limiting the radiation to a specific tumor has been difficult, with the result that radiation doses were kept low to protect healthy organs. This also meant numerous sessions spread over months. Based on all of this, radiation has not typically been a first line of treatment for pancreatic cancer.
But science marches on! Modern technology has enabled high-precision lasers that can track tumors even while they move. Basically, the laser triangulates the cancer’s position by focusing on microscopic particles of gold that were previously injected to the tumor site. (No, my intrinsic value won’t change noticeably just because my tumor is gold-plated. The key word here is “microscopic”.)
This new laser, which by the way is called CyberKnife—presumably by a marketer, it’s too trendy to have been named by a scientist—allows much higher doses of radiation, since the target area is so precise. This in turn means only 5 sessions over 5 days instead of months of zapping. The whole process is known as SBRT, which in any rational universe would obviously stand for Special Beams to Reduce Tumors, but which in our mundane existence actually stands for Stereotactic Body RadioTherapy. (Presumably named by a scientist, not a marketer.)
For more details, check out this CyberKnife patient education video.
Even with these improvements, external beam treatment is not appropriate for liver cancer. The liver is apparently the Laura Wingfield of organs, too delicate for high-radiation SBRT. Luckily, its unique physiology presents an alternative treatment option: radioembolization.
Had I attended 9th grade in the U.S. instead of studying botany and economic geography in Russian, I might have learned that the liver is unusual for getting its supply of blood from two vessels: the portal vein and the hepatic artery. The burden is not equal; the portal vein carries 75% of blood to the liver. However—and this is where things get interesting—liver tumors get 90% of their blood from the other vessel (the hepatic artery).
What does that mean? It means that, rather than trying to aim an external source of radiation, doctors can actually inject radioactive particles into the hepatic artery. The particles travel directly to the tumors and get busy killing them, while healthy liver tissue continues to get radiation-free blood via the portal vein. After the particles (yttrium-90, if you’re curious) are in place, the hepatic artery can even be blocked to prevent the radioactive particles from traveling without significantly reducing blood flow to the rest of the liver.
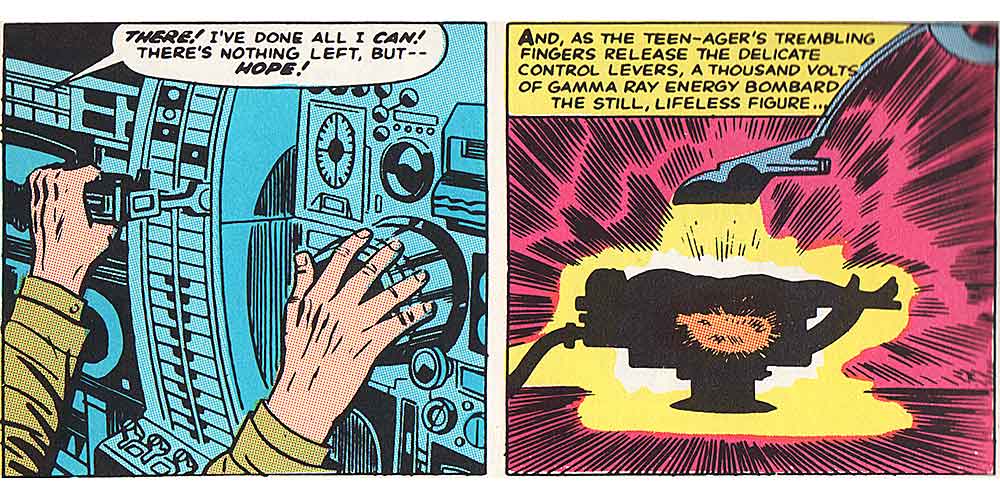
Pretty spiffy, no? The radiation typically extends just a few millimeters, so nothing other than the tumors should be affected. Still, I was cautioned not to hug small children for a few days after treatment. So instead of turning into Spider-Man or the Incredible Hulk (much to the kids’ dismay), my only superpowers will be avoiding toddlers and triggering Geiger counters.
For more details, check out this video on radioembolization and the yttrium-90 microspheres.

This looks like a job for…
This looks like a job for… Super-Hermit! 😉
Super powers
what I wouldn't give for a super power to avoid certain adults!